A mastoidectomy is a surgical procedure that involves the removal of part or all of the mastoid bone, which is located behind the ear. It's important to consult with an ENT specialist or otolaryngologist to discuss the benefits, risks, and expected outcomes of a mastoidectomy based on your specific condition.
Mastoidectomy (mastoid surgery) is a surgical procedure performed to treat various conditions affecting the mastoid bone, which is located behind the ear. This intricate procedure involves the removal of infected or damaged tissues within the mastoid bone, often necessary to address chronic ear infections, cholesteatoma, or other related complications. In this article, we will delve into the details of Mastoidectomy, exploring its purpose, techniques, recovery process, and potential benefits.
Mastoidectomy and Tympanoplasty
Tympano mastoidectomy:
In some cases, tympanoplasty with mastoidectomy and may be performed together. This approach allows the surgeon to address both the infection or disease within the mastoid bone and any associated eardrum perforation or middle ear damage in a single surgery. Performing both procedures simultaneously can help achieve better outcomes, especially when the conditions are interconnected or when addressing the underlying cause of the ear problem requires a comprehensive approach.
Purpose of Mastoidectomy Surgery
Mastoidectomy serves both diagnostic and therapeutic purposes. It is primarily performed to treat chronic ear infections that have not responded to non-surgical interventions, such as antibiotics. Additionally, mastoidectomy is employed to address cholesteatoma, a non-cancerous growth that can develop in the middle ear, causing hearing loss, balance problems, and potential complications like infection and damage to surrounding structures.
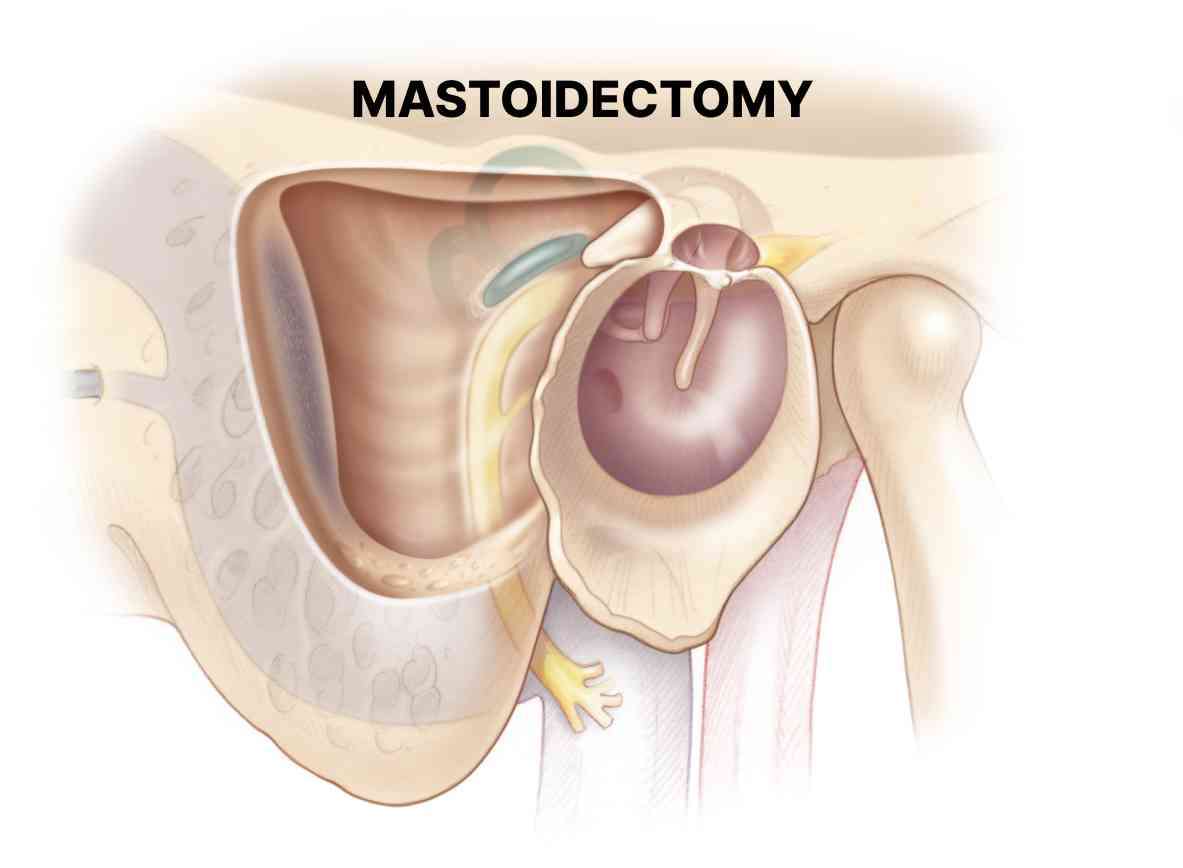
Procedure and Techniques
The mastoidectomy procedure is typically conducted under general anesthesia, ensuring the patient's comfort and relaxation throughout the surgery. The surgeon makes an incision behind the ear, exposing the mastoid bone. The bone is then carefully drilled away to create an opening leading to the middle ear. This allows the surgeon to access and remove the infected or damaged tissues, clear any accumulated fluid, and address any underlying issues, such as cholesteatoma. Depending on the severity of the condition, the surgeon may perform different types of mastoidectomy, including simple, modified radical, or radical mastoidectomy. These variations vary in the extent of tissue removal and reconstruction needed, with the aim of preserving hearing function while effectively treating the underlying problem. Ear discharge after mastoidectomy
Ear discharge after mastoidectomy can occur for various reasons and may require medical attention. Here are a few possible explanations for ear discharge following mastoidectomy: Normal Healing Process: In the initial days or weeks after mastoidectomy, it is common to have some mild ear discharge, which is typically a combination of blood, surgical fluids, and mucus. This discharge is part of the normal healing process and should decrease over time. It is important to follow your surgeon's instructions on how to clean and care for the ear during this healing phase. Infection: Ear discharge can be a sign of infection, especially if it is accompanied by increased pain, swelling, redness, foul odor, or fever. Infections can occur in the surgical site or the middle ear. Prompt medical attention is necessary to diagnose and treat any infection to prevent further complications. Persistent or Recurrent Cholesteatoma: Cholesteatoma is a condition characterized by the growth of abnormal skin cells in the middle ear. Despite mastoidectomy, cholesteatoma can recur or persist, leading to ongoing ear discharge. Further evaluation and treatment by an ear, nose, and throat specialist are required if cholesteatoma is suspected. Cerebrospinal Fluid Leak: In rare cases, a mastoidectomy can inadvertently damage the covering of the brain (dura), resulting in a cerebrospinal fluid (CSF) leak. CSF leakage may cause clear or watery discharge from the ear, which may increase when bending over or straining. A CSF leak requires immediate medical attention to prevent infection and further complications.
Purpose of Mastoidectomy Surgery
Mastoidectomy serves both diagnostic and therapeutic purposes. It is primarily performed to treat chronic ear infections that have not responded to non-surgical interventions, such as antibiotics. Additionally, mastoidectomy is employed to address cholesteatoma, a non-cancerous growth that can develop in the middle ear, causing hearing loss, balance problems, and potential complications like infection and damage to surrounding structures.
Procedure and Techniques
The mastoidectomy procedure is typically conducted under general anesthesia, ensuring the patient's comfort and relaxation throughout the surgery. The surgeon makes an incision behind the ear, exposing the mastoid bone. The bone is then carefully drilled away to create an opening leading to the middle ear. This allows the surgeon to access and remove the infected or damaged tissues, clear any accumulated fluid, and address any underlying issues, such as cholesteatoma.
Depending on the severity of the condition, the surgeon may perform different types of mastoidectomy, including simple, modified radical, or radical mastoidectomy. These variations vary in the extent of tissue removal and reconstruction needed, with the aim of preserving hearing function while effectively treating the underlying problem.
Ear discharge after mastoidectomy
Ear discharge after mastoidectomy can occur for various reasons and may require medical attention. Here are a few possible explanations for ear discharge following mastoidectomy:
Normal Healing Process: In the initial days or weeks after mastoidectomy, it is common to have some mild ear discharge, which is typically a combination of blood, surgical fluids, and mucus. This discharge is part of the normal healing process and should decrease over time. It is important to follow your surgeon's instructions on how to clean and care for the ear during this healing phase.
Infection: Ear discharge can be a sign of infection, especially if it is accompanied by increased pain, swelling, redness, foul odor, or fever. Infections can occur in the surgical site or the middle ear. Prompt medical attention is necessary to diagnose and treat any infection to prevent further complications.
Persistent or Recurrent Cholesteatoma: Cholesteatoma is a condition characterized by the growth of abnormal skin cells in the middle ear. Despite mastoidectomy, cholesteatoma can recur or persist, leading to ongoing ear discharge. Further evaluation and treatment by an ear, nose, and throat specialist are required if cholesteatoma is suspected.
Cerebrospinal Fluid Leak: In rare cases, a mastoidectomy can inadvertently damage the covering of the brain (dura), resulting in a cerebrospinal fluid (CSF) leak. CSF leakage may cause clear or watery discharge from the ear, which may increase when bending over or straining. A CSF leak requires immediate medical attention to prevent infection and further complications.
Post-operative management plays a crucial role in the successful recovery of patients who have undergone mastoidectomy for mastoiditis. Here are some key aspects of post-operative care: Wound Care: Following mastoidectomy, it is essential to keep the surgical wound clean and dry to prevent infection. The surgeon will provide specific instructions on how to care for the wound, including how to clean it and change dressings, if necessary. It is important to follow these instructions diligently to promote proper healing. Pain Management: Pain and discomfort are common after mastoidectomy. The surgeon may prescribe pain medications to help manage post-operative pain. It is important to take the medications as directed and report any severe or persistent pain to the healthcare provider. Antibiotics: Antibiotics may be prescribed after mastoidectomy to prevent or treat any post-operative infection. It is crucial to take the antibiotics as prescribed and complete the full course, even if symptoms improve. Report any signs of infection, such as increased pain, swelling, redness, or discharge, to the healthcare provider promptly. Activity Restrictions: During the initial recovery period, it is important to avoid activities that can increase pressure in the ear or disrupt the healing process. This may include avoiding activities such as air travel, scuba diving, swimming, or strenuous exercises. Follow the surgeon's instructions regarding activity restrictions and gradually resume normal activities as advised. Follow-Up Visits: Regular follow-up visits with the surgeon are essential to monitor the healing progress and ensure proper recovery. These visits allow the surgeon to assess the surgical site, address any concerns or complications, and make any necessary adjustments to the treatment plan. Ear Care: Proper ear care is important after mastoidectomy. Avoid inserting anything into the ear, including cotton swabs, as it can disrupt the healing process and increase the risk of infection. The surgeon may provide specific instructions on how to clean the ear, if necessary, using appropriate techniques or solutions. Hearing Rehabilitation: In some cases, mastoidectomy may affect hearing function. The surgeon will discuss any changes in hearing and recommend appropriate rehabilitation options, such as hearing aids or other devices, if needed. It is important to follow up with the recommended hearing rehabilitation plan to optimize hearing outcomes. Precautions and Complications: Be aware of potential complications associated with mastoidectomy, such as infection, bleeding, facial nerve injury, dizziness, or hearing loss. Report any concerning symptoms or complications to the healthcare provider promptly.
Post-operative management plays a crucial role in the successful recovery of patients who have undergone mastoidectomy for mastoiditis. Here are some key aspects of post-operative care:
Wound Care: Following mastoidectomy, it is essential to keep the surgical wound clean and dry to prevent infection. The surgeon will provide specific instructions on how to care for the wound, including how to clean it and change dressings, if necessary. It is important to follow these instructions diligently to promote proper healing.
Pain Management: Pain and discomfort are common after mastoidectomy. The surgeon may prescribe pain medications to help manage post-operative pain. It is important to take the medications as directed and report any severe or persistent pain to the healthcare provider.
Antibiotics: Antibiotics may be prescribed after mastoidectomy to prevent or treat any post-operative infection. It is crucial to take the antibiotics as prescribed and complete the full course, even if symptoms improve. Report any signs of infection, such as increased pain, swelling, redness, or discharge, to the healthcare provider promptly.
Activity Restrictions: During the initial recovery period, it is important to avoid activities that can increase pressure in the ear or disrupt the healing process. This may include avoiding activities such as air travel, scuba diving, swimming, or strenuous exercises. Follow the surgeon's instructions regarding activity restrictions and gradually resume normal activities as advised.
Follow-Up Visits: Regular follow-up visits with the surgeon are essential to monitor the healing progress and ensure proper recovery. These visits allow the surgeon to assess the surgical site, address any concerns or complications, and make any necessary adjustments to the treatment plan.
Ear Care: Proper ear care is important after mastoidectomy. Avoid inserting anything into the ear, including cotton swabs, as it can disrupt the healing process and increase the risk of infection. The surgeon may provide specific instructions on how to clean the ear, if necessary, using appropriate techniques or solutions.
Hearing Rehabilitation: In some cases, mastoidectomy may affect hearing function. The surgeon will discuss any changes in hearing and recommend appropriate rehabilitation options, such as hearing aids or other devices, if needed. It is important to follow up with the recommended hearing rehabilitation plan to optimize hearing outcomes.
Precautions and Complications: Be aware of potential complications associated with mastoidectomy, such as infection, bleeding, facial nerve injury, dizziness, or hearing loss. Report any concerning symptoms or complications to the healthcare provider promptly.
Mastoidectomy offers several significant benefits to patients suffering from chronic ear infections or cholesteatoma. These include: a. Relief from Symptoms: By removing infected or damaged tissues, mastoidectomy helps alleviate the symptoms associated with chronic ear infections, such as pain, discharge, hearing loss, and dizziness. It can also prevent the spread of infection to other parts of the ear or nearby structures. b. Prevention of Complications: Untreated chronic ear infections or cholesteatoma can lead to severe complications, including hearing loss, balance problems, facial nerve paralysis, meningitis, or brain abscess. mastoidectomy effectively addresses these issues, minimizing the risk of further complications and improving overall health outcomes. c. Improved Quality of Life: By resolving chronic ear infections and related issues, mastoidectomy can significantly enhance a patient's quality of life. Restored hearing, reduced pain and discomfort, and the elimination of recurrent infections can have a profound impact on communication, social interactions, and overall well-being. Different types of mastoidectomy surgery: Simple Mastoidectomy: Simple mastoidectomy involves the removal of infected or damaged tissue from the mastoid air cells, without disturbing the structures of the middle ear. It is commonly performed to treat chronic ear infections that have not responded to other treatments. This procedure aims to improve the drainage and ventilation of the middle ear, thereby reducing the risk of recurrent infections. Modified Radical Mastoidectomy:Modified radical mastoidectomy involves the removal of infected or diseased tissue from the mastoid bone and part of the middle ear structures. This procedure is typically performed when the disease has extended beyond the mastoid air cells into the middle ear, potentially affecting the ossicles (tiny bones involved in hearing). Procedure of Modified Radical Mastoidectomy: The surgeon removes the affected tissue, opens up the mastoid cavity, and reconstructs the middle ear structures to restore hearing function. Radical Mastoidectomy: Radical mastoidectomy is the most extensive type of mastoidectomy. It involves the complete removal of the mastoid air cells, the diseased tissue within the middle ear, and sometimes the eardrum. This procedure is reserved for cases where the disease has spread significantly and poses a risk to critical structures, such as the facial nerve or inner ear. Reconstruction of the middle ear is often necessary to preserve hearing. Canal Wall-Up (Closed) Mastoidectomy:Canal wall-up mastoidectomy involves the removal of infected or damaged tissue from the mastoid bone while leaving the external ear canal intact. This procedure is typically performed to address cholesteatoma, a non-cancerous growth that can erode bone and cause complications. Procedure of Canal Wall-Up (Closed) Mastoidectomy: The surgeon removes the diseased tissue and reconstructs the middle ear structures while preserving the natural ear canal. Procedure of canal wall up mastoidectomy: Canal Wall-Down (Open) Mastoidectomy: This procedure is performed in cases where extensive disease or recurrent cholesteatoma requires ongoing monitoring and care. The opening allows for regular cleaning and inspection of the mastoid cavity to prevent future infections or complications. Procedure of Canal Wall-Down (Open) Mastoidectomy: Canal wall-down mastoidectomy involves the removal of infected or diseased tissue from the mastoid bone and the creation of a permanent opening (mastoid cavity) between the middle ear and the external ear canal.
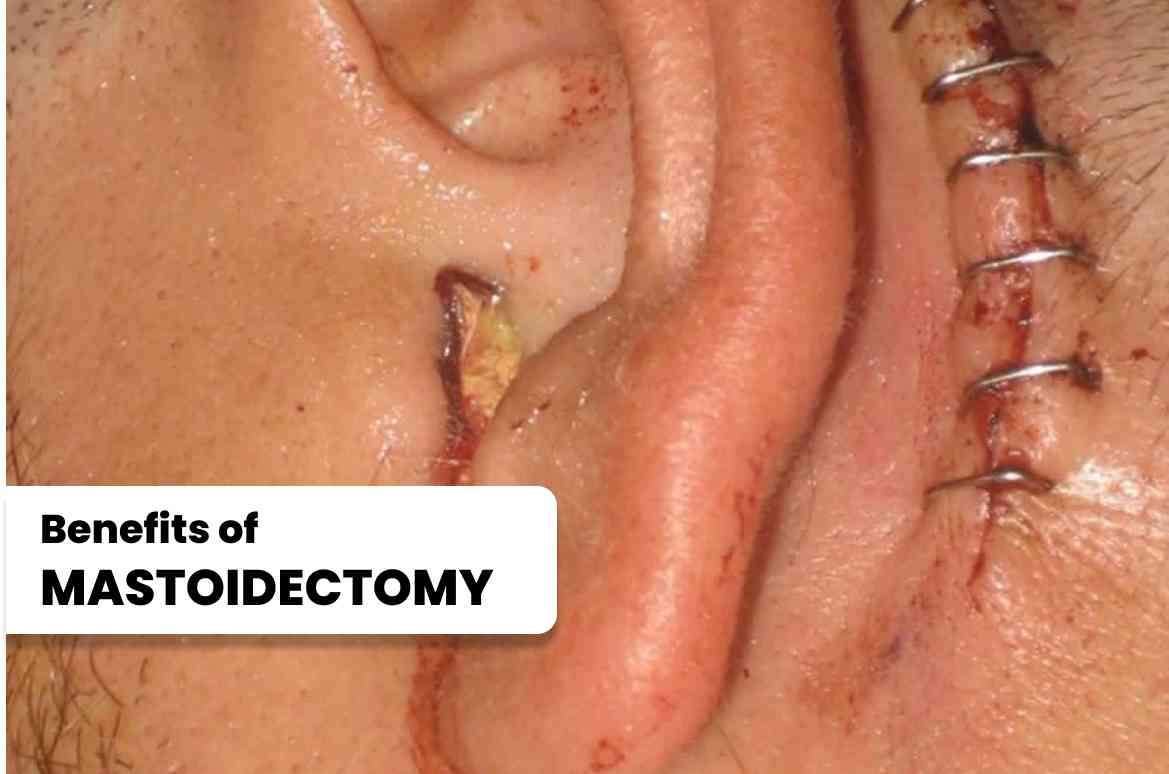
Mastoidectomy offers several significant benefits to patients suffering from chronic ear infections or cholesteatoma. These include:
a. Relief from Symptoms: By removing infected or damaged tissues, mastoidectomy helps alleviate the symptoms associated with chronic ear infections, such as pain, discharge, hearing loss, and dizziness. It can also prevent the spread of infection to other parts of the ear or nearby structures.
b. Prevention of Complications: Untreated chronic ear infections or cholesteatoma can lead to severe complications, including hearing loss, balance problems, facial nerve paralysis, meningitis, or brain abscess. mastoidectomy effectively addresses these issues, minimizing the risk of further complications and improving overall health outcomes.
c. Improved Quality of Life: By resolving chronic ear infections and related issues, mastoidectomy can significantly enhance a patient's quality of life. Restored hearing, reduced pain and discomfort, and the elimination of recurrent infections can have a profound impact on communication, social interactions, and overall well-being.
Different types of mastoidectomy surgery:
Simple Mastoidectomy: Simple mastoidectomy involves the removal of infected or damaged tissue from the mastoid air cells, without disturbing the structures of the middle ear. It is commonly performed to treat chronic ear infections that have not responded to other treatments. This procedure aims to improve the drainage and ventilation of the middle ear, thereby reducing the risk of recurrent infections.
Modified Radical Mastoidectomy:Modified radical mastoidectomy involves the removal of infected or diseased tissue from the mastoid bone and part of the middle ear structures. This procedure is typically performed when the disease has extended beyond the mastoid air cells into the middle ear, potentially affecting the ossicles (tiny bones involved in hearing).
Procedure of Modified Radical Mastoidectomy: The surgeon removes the affected tissue, opens up the mastoid cavity, and reconstructs the middle ear structures to restore hearing function.
Radical Mastoidectomy: Radical mastoidectomy is the most extensive type of mastoidectomy. It involves the complete removal of the mastoid air cells, the diseased tissue within the middle ear, and sometimes the eardrum. This procedure is reserved for cases where the disease has spread significantly and poses a risk to critical structures, such as the facial nerve or inner ear. Reconstruction of the middle ear is often necessary to preserve hearing.
Canal Wall-Up (Closed) Mastoidectomy:Canal wall-up mastoidectomy involves the removal of infected or damaged tissue from the mastoid bone while leaving the external ear canal intact. This procedure is typically performed to address cholesteatoma, a non-cancerous growth that can erode bone and cause complications.
Procedure of Canal Wall-Up (Closed) Mastoidectomy:
The surgeon removes the diseased tissue and reconstructs the middle ear structures while preserving the natural ear canal.
Procedure of canal wall up mastoidectomy:
Canal Wall-Down (Open) Mastoidectomy: This procedure is performed in cases where extensive disease or recurrent cholesteatoma requires ongoing monitoring and care. The opening allows for regular cleaning and inspection of the mastoid cavity to prevent future infections or complications.
Procedure of Canal Wall-Down (Open) Mastoidectomy: Canal wall-down mastoidectomy involves the removal of infected or diseased tissue from the mastoid bone and the creation of a permanent opening (mastoid cavity) between the middle ear and the external ear canal.
Please Wait..